PRK Complications
A lucrative business for ophthalmologists, PRK is a harmful, unnecessary eye surgery. PRK preceded LASIK, but then fell out of favor as LASIK was introduced. From the ophthalmologist-businessman’s perspective, LASIK did not require as much chair time as PRK, and LASIK was more marketable than PRK. After widespread problems from LASIK came to light, PRK was reintroduced under new marketing terms such as “advanced surface ablation” and LASEK. We believe PRK and LASEK will someday be abandoned once and for all to the junk heap of refractive surgeries.
What is PRK?
PRK stands for photorefractive keratectomy. Like LASIK, the goal of PRK is to reduce or eliminate the need for glasses or contact lenses. PRK is similar to LASIK surgery in that a laser is used to burn away corneal tissue, which changes how light rays focus on the retina. The primary difference is that, in LASIK, a corneal flap is made with a blade or a laser to expose the corneal stroma to the laser. In PRK, the surface layer of the cornea – the epithelium – is scraped away or otherwise removed without cutting a flap. Epithelial cells regenerate over a period of several days after PRK; however, Bowman’s membrane, which plays a vital role in health of the cornea, is permanently destroyed in the ablated zone. Some ophthalmologists speculate that permanent destruction of Bowman’s membrane during PRK may lead to late-onset complications, as Bowman’s membrane is a protective barrier between the environment and the corneal stroma.
What about LASEK?
There is very little difference between PRK and LASEK. In the original PRK method, the surface of the cornea – the epithelium – is removed (destroyed) mechanically to expose the cornea prior to laser ablation. In LASEK, the epithelium is softened with an alcohol solution and then lifted to expose the cornea. In LASEK, after laser treatment the epithelium is returned to position. This may initially sound like a better method than destroying the epithelium, but many surgeons oppose it. Retaining damaged epithelium has been associated with post-operative complications. Asking the question “which is better, PRK or LASEK?”, may be like asking, “is it better to break my arm with a baseball bat or a sledgehammer?”
What are the risks of PRK?
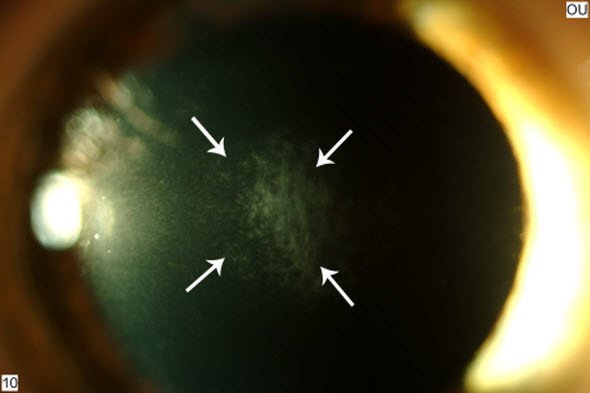
Haze (scarring) is a common complication of PRK. To reduce risk of haze, many surgeons currently use a toxic substance called MMC during PRK. MMC is a chemotherapy agent which results in cell death and is not FDA-approved for use with PRK. MMC has been reported to have long-term adverse effects on the eye. Here’s a link to a collection of research articles on MMC.
Pain, haze, chronic dry eyes, regression, and night vision problems are the most common complaints after PRK and LASEK. All eyes experience persistent, accelerated loss of corneal cells after PRK.
PROBLEMS AFTER PRK/LASEK? File a MedWatch report with the FDA online. Alternatively, you may call FDA at 1-800-FDA-1088 to report by telephone, download the paper form and either fax it to 1-800-FDA-0178 or mail it to the address shown at the bottom of page 3, or download the MedWatcher Mobile App for reporting LASIK problems to the FDA using a smart phone or tablet.
Patients with LASIK complications are invited to join the discussion on Facebook